Makoplasty Robotic Partial Knee Replacement Best for One Compartment Disease
While Makoplasty parts can be combined in several different configurations, by far the most common is to resurface only one compartment. The one compartment most commonly resurfaced is the medial compartment of the knee.
Medial knee is the time tested application with predictably great outcomes. This procedure has been dramatically improved upon using Robotic Technology.
In my opinion, lateral uni compartmental application works well when your surgeon is able to incorporate accurate implant placement using Makoplasty Robotics and Computer Balancing and CT mapping technology.
 |
| Xray of Medial Mako (most common construct) |
| Bicompartmental Mako components (No patellar button shown and 2 options for tibial resurfacing shown) |
 |
| Cartoon of Bicompartmental Mako (no patellar button) |
Bicompartmental Knee Resurfacing:
In my hands, bicompartmental use is a less desirable construct. If two or more compartments are arthritic Dr. T. will usually recommend Total Knee Replacement. Another bicompartmental construct is to resurface the medial and lateral compartments, leaving healthy patella. This is rarely done and no xray image was able to be found on line to even demonstrate the appearance of this.
 |
| Xray of Bicompartmental Mako (patellofemoral + medial uni) |
Makoplasty Unicompartmental Knee Mimics Natural Knee
Dr. Tarlow attended a course titled “Update on Unicondylar Knee Replacement” this past week at the annual meeting of the American Academy of Orthopedic Surgeons.

The appeal of the unicompartmental or partial knee replacement also known as Makoplasty can be summarized in the following thoughts.
Makoplasty replaced knees compared to Total Knee Replacement:
- Retain more normal knee tissue – including the ACL and PCL ligaments
- There is less bone resection
- Smaller incisions
- Less pain/quicker recovery
- improved, often times normal knee motion
- Less expensive
Makoplasty Partial Knee Resurfacing Shown To Be Best Surgical Method
Study finds MAKOplasty® Partial Knee Resurfacing Offers Lower Post-Op Pain, Improved Knee Function
- Lower post-operative pain from day one up to 8 weeks after surgery
- More accurate implant placement
- Twice as many patients with improved knee functionality (57% vs. 26%) based on American Knee Society Scores
Makoplasty Knee Surgery and Home In One Day-Outpatient Partial Knee Replacement
 |
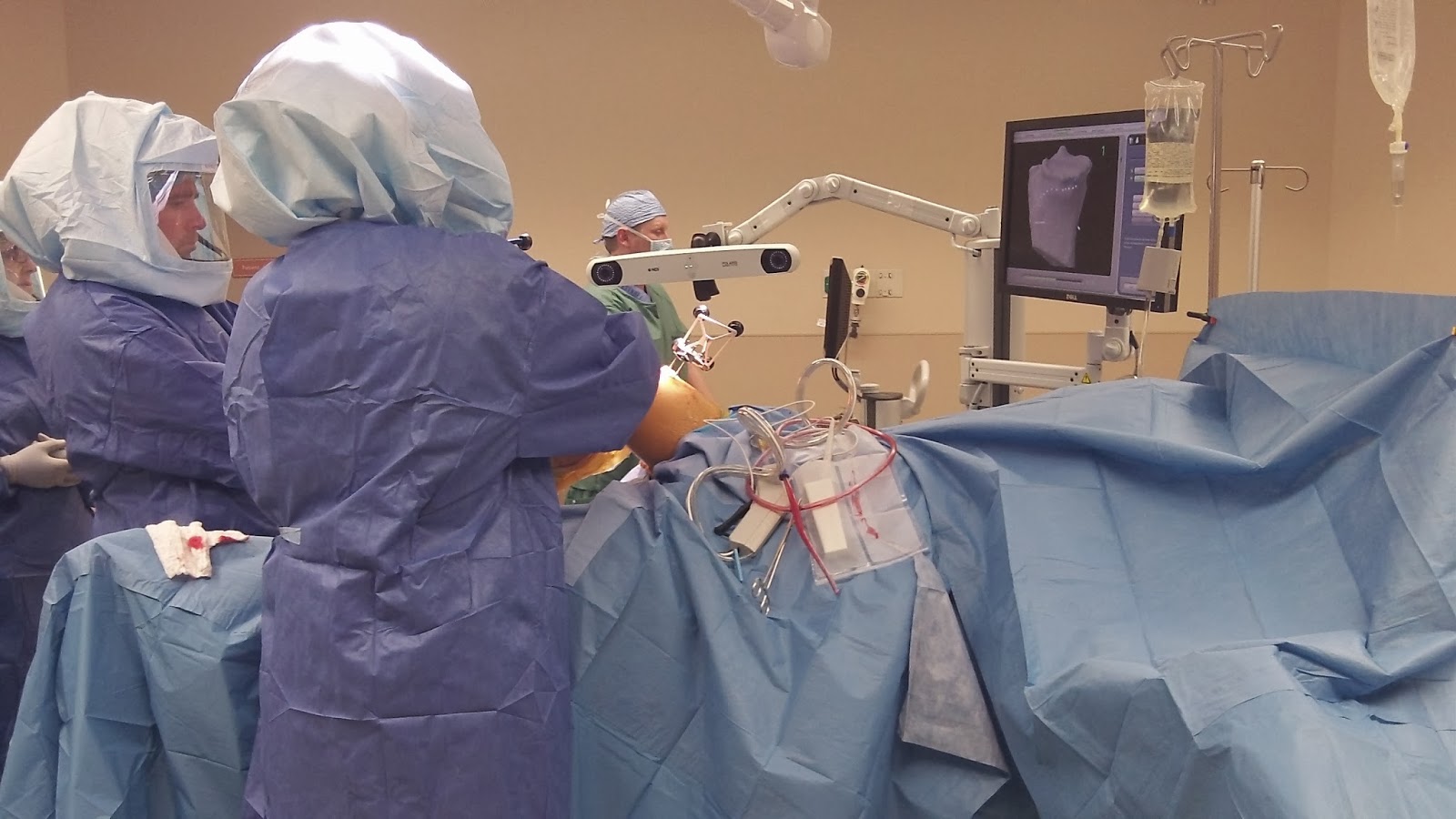
| Dr. Tarlow team performing Makoplasty |
Stefan D. Tarlow, M.D., Knee Surgeon with Advanced Knee Care, P.C. has posted a new video with an overview showing how Makoplasty, a partial knee replacement procedure using robotic technology can be performed as an outpatient. Click here to watch the 4 minute video.
Makoplasty – Partial Knee Replacement – Home the Same Day
Scottsdale Healthcare Thompson Peak acquired a Mako RIO system in Janaury, 2011. Since that time Dr. Stefan Tarlow has performed over 180 procedures, more than any other orthopedic surgeon in Arizona. Dr. Tarlow is Arizona’a most practiced and well-versed Makoplasty surgeon. Not content with status quo, he and his team continue to innovate and improve on the technique.Our team of Surgeons, Nurses and Anesthesiologists have continued to refine our delivery of care for our surgical patients. This is particularly evident in the patients undergoing partial knee replacement using the robotic technology known as Makoplasty.
Today’s standard delivery of care has evolved to outpatient day surgery
due to improved surgical efficiency, saphenous nerve block (little to no motor weakness compared to femoral nerve block), and recovery room pain management with short acting opiods (Fentanyl). Together these modifications allow many patients to go home directly from recovery room.